This article was contributed by Dr Hannah Bellsham-Revell, Paediatric Cardiology consultant at Evelina Children’s Hospital
In this post we will discuss our approach to an unwell newborn baby. Sepsis is ALWAYS the major concern here and this cannot be emphasised enough… however, many of us will be much less confident in the diagnosis and management of the various differential diagnosis that can ‘mimic’ sepsis in a collapsed infant. In particular, we’re going to concentrate on congenital cardiac disease and think about how the presenting clinical features can help guide us to a diagnosis.
A 10 day old baby girl presents to ED:
Poor feeding for the last 48hrs, progressively poor colour and difficulty breathing over the last few hours. On assessment she is:
Grey and floppy, moaning, just rousable
Grunting, tachypnoeic with recession and nasal flaring, unrecordable saturations
CRT 5s centrally, 8s peripherally, weak pulses with unrecordable BP, HR 180, Temp 35.5oC
The differential diagnosis at this point is
-
- Sepsis
- Sepsis
- SEPSIS!
- Cardiac
- Metabolic
- Cerebral bleed (although less common now since the introduction of vitamin K injections at birth)
Initial management is similar WHATEVER the diagnosis… ABC…resuscitation… broad spectrum antibiotics. Then, a search for clues begins. What aspects of the history and examination will point you towards a particular diagnosis? If you don’t consider other diagnoses, you won’t find them…
Sepsis |
Cardiac |
Metabolic |
Cerebral bleed |
| Fever (although not always seen in neonates)Infectious signs – rash, cough, vomiting etc | Sweating/breathlessness with feedsProgressive decrease in feeding
Colour changes (although blue/hands feet can be normal in a newborn) Family history of congenital cardiac disease |
Family history of neonatal deathsConsanguinity |
Not had vitamin K Inconsistent history Other injuries Consider NAI |
To keep things focused, we are going to brush over the sepsis bit for once and concentrate on the cardiac causes of neonatal collapse.
The pathologies that can cause circulatory collapse in an infant can be divided into 4 groups.

Duct dependent conditions
i.e. The baby’s circulation relies on the ductus arteriosus (‘the duct’) still being open. As it starts to close, trouble begins.
Systemic duct dependent: Left heart obstruction where the systemic circulation only receives sufficient blood from ductal shunting from the pulmonary artery to the aorta.
Pulmonary duct dependent: Right heart obstruction where the pulmonary circulation only receives sufficient blood from ductal shunting from the aorta to the pulmonary artery.
Mixing dependent: Obligatory right to left shunt (TAPVD) or reverse parallel circulations (transposition of the great arteries)
Duct dependent systemic lesions – HLHS, CoA, critical AS
Clinically these can be tricky! The baby:
- May or may not have a murmur
- May or may not be desaturated
- May or may not have hepatomegaly
(cheers physiology, few clues there!) The index of suspicion for a duct dependent problem rises if the timing of the presentation fits – the duct usually closes between day 2-7 – but beware the late closing duct! In duct dependent coarctation of the aorta, post-ductal saturations might be lower than pre-ductal while the duct is open (as the duct is shunting deoxygenated blood to the aorta). As the duct shuts, the post-ductal saturations will increase but blood pressure and peripheral pulses will decrease. There will be a blood pressure and pulse differential in coarctation (pre-ductal higher than post-ductal). In critical aortic stenosis and hypoplastic left heart syndrome, ALL pulses and BP will be weak.
If the circulation is failing as the duct closes, the organs will not be well perfused – so you may see:
- Acidosis (tissue hypoperfusion)
- Deranged U&Es, reduced urine output (renal hypoperfusion)
- Abnormal LFTs, coagulopathy (liver hypoperfusion)
- NEC (gut ischaemia)
- Seizures (cerebral hypoperfusion)
Duct dependent pulmonary lesions – TA, PA, critical PS, severe TOF
- Desaturation will be present
- There may or may not be a murmur…
- No blood pressure or pulse differential (unless there is left heart obstruction too)Acidosis and end organ damage (as above) might occur, but this will be from hypoxia rather than hypoperfusion. As babies have high fetal haemoglobin levels (which as you remember has high affinity for oxygen), they often ‘tolerate’ cyanosis surprisingly well
Mixing Dependent:
- May or may not have a murmur
- Transposition of the great arteries (TGA): the right arm (pre-ductal) saturations will be lower than post-ductal (feet)
NON duct dependent conditions
In these babies, it makes little difference whether or not the ductus arteriosus is open or closed – their circulation is severely abnormal (for example a common arterial trunk or anomalous pulmonary venous drainage) and they are not reliant on the shunting of blood via the duct.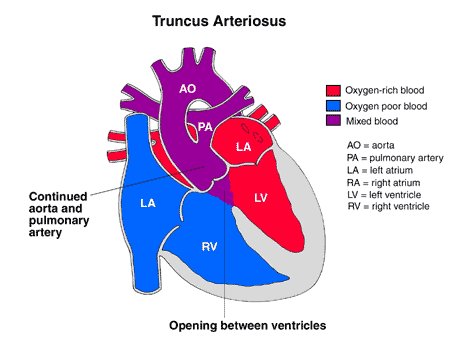
Common arterial trunk (truncus arteriosus): As the pulmonary vascular resistance falls, torrential pulmonary blood flow floods the lungs. The baby will develop respiratory signs (tachypnoea, increased work of breathing), hepatomegaly and systemic underperfusion (which leads to acidosis and end organ effects). Usually there is a loud murmur (from truncal regurgitation/stenosis, along with the VSD)
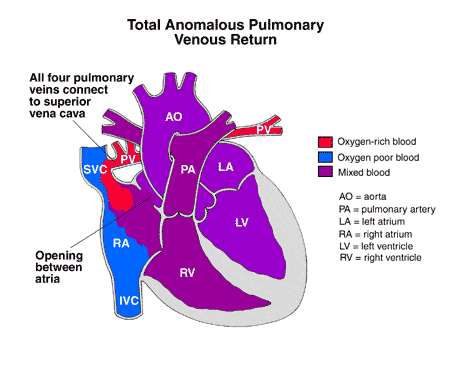 Total Anomalous pulmonary venous drainage (rare!): Total anomalous pulmonary venous drainage usually presents as a neonate or infant. (partial anomalous pulmonary venous drainage may be a later incidental finding). The quirk of anatomy here is that pulmonary veins do not drain into the left atrium – instead they empty into the vena cava – leading to pulmonary congestion and an underfilled left heart. These babies present with respiratory signs due to their soggy lungs (tachypnoea, increased work of breathing) and systemic underperfusion (acidosis, end organ effects). Unhelpfully, there may or may not be a murmur, but there is likely to be a palpable liver due to right heart congestion. Obstruction to pulmonary venous return – even in partial anomalous drainage – can have an impact. Infracardiac TAPVD is most often obstructed, but supra and intracardiac TAPVD can also be obstructed.
Total Anomalous pulmonary venous drainage (rare!): Total anomalous pulmonary venous drainage usually presents as a neonate or infant. (partial anomalous pulmonary venous drainage may be a later incidental finding). The quirk of anatomy here is that pulmonary veins do not drain into the left atrium – instead they empty into the vena cava – leading to pulmonary congestion and an underfilled left heart. These babies present with respiratory signs due to their soggy lungs (tachypnoea, increased work of breathing) and systemic underperfusion (acidosis, end organ effects). Unhelpfully, there may or may not be a murmur, but there is likely to be a palpable liver due to right heart congestion. Obstruction to pulmonary venous return – even in partial anomalous drainage – can have an impact. Infracardiac TAPVD is most often obstructed, but supra and intracardiac TAPVD can also be obstructed.
images: Children’s Hospital of Wisconsin
Arrhythmias
Tachycardia in the neonate may be of a variety of origins, ventricular tachycardias are extremely rare, with most arrhythmias originating in the atria or in abnormalities of the conduction system. As they are often well tolerated, diagnosis may be delayed until the baby collapses. Careful analysis of the ECG and discussion with cardiologists is essential. Congenital complete heart block can be seen in neonates. The child may be sick and hydropic, or it may be an incidental finding. Management depends on the clinical condition of the child. If the mum has an autoimmune disease – or has anti-Ro/La antibodies (with SLE) – this increases the risk of neonatal arrythmias.
Cardiomyopathy
Put simply, this is dysfunction of the myocardium. We can categorise it as dilated, hypertrophic or restrictive:
Dilated cardiomyopathy may be congenital, metabolic, infectious or related to a tachyarrhythmia.
- May or may not have a murmur
- May have gallop rhythm
- Hepatomegaly
- Varying ECG abnormalities may be seen (ischaemia may raise the question of myocarditis or an anomalous coronary artery origin)
- Investigations for causes are essential as some are reversible
Hypertrophic cardiomyopathy may be congenital or metabolic, but can also be seen in babies of diabetic mothers.
- May have a murmur (usually from outflow tract obstruction)
- May have hepatomegaly
- Very large complexes on ECG. If you see a short PR interval in association with giant QRS complexes then suspect a storage disease (e.g. Pompes)
Restrictive cardiomyopathy is extremely rare, but usually carries a very poor prognosis.
- May have a murmur (usually from mitral and/or tricuspid regurgitation)
- May have hepatomegaly
- Atrial enlargement on ECG
- Arrhythmias
When might different cardiac lesions present?
Another approach to differentiating possible cardiac causes of collapse in infants is to divide them by time of presentation. Certain lesions typically present at particular times – and this can be very helpful in diagnosis and management.
| Timing | Differentials |
| Immediately after birth– usually related to atrial obstruction | Obstructed pulmonary venous return– Obstructed TAPVD
– HLHS with intact/highly restrictive atrial septum Obstructed mixing – TGA with intact/highly restrictive atrial septum Myocarditis, cardiomyopathy, arrhythmia PPHN |
| Day 2-7- Usually related to ductal closure | Duct dependent systemic circulation- HLHS, CoA, critical AS
Duct dependent pulmonary circulation – TA, PA, critical PS, severe TOF Huge shunts as the PVR falls (large aortopulmonary window, common arterial trunk) Myocarditis, cardiomyopathy, arryhthmia |
| Within 28 days | Majority of atrial/ductal dependent lesions with delayed closure of the duct/PFO or that are not totally dependent– TGA, CoA, critical PS/AS, TOF
Conditions which worsen as the pulmonary blood flow increases – TAPVD, left heart obstructive lesions – Very large shunts (large PDA, AVSD, VSD) Myocarditis, cardiomyopathy, arrhythmia |
| 4-6 weeks | As the pulmonary vascular resistance falls and pulmonary blood flow increases– Shunts: VSD, PDA
– TAPVD – Milder CoA/AS – TOF Myocarditis, cardiomyopathy, arrhythmia |
Key points
The initial treatment of a collapsed neonate is similar, whatever the cause.
History and examination might point you in the direction of the diagnosis – always consider a wider differential than ‘just’ sepsis.
Response to treatment may help to differentiate the cause
Beware a mixed picture! For example – Sepsis AND a cardiac condition; Complex CHD with left obstruction AND large shunt, etc
Seek advice at all stages if unsure

Pingback: Neonatal Cardiology Quiz
very useful presentation as I have not been exposed to these diseases yet in practice, that would refresh the memory and act in structured manner when time comes and be in front of these unwell babies. Many Thanks
Bonjour merci d ‘exposer ce problème de pratique ,cependant je souhaiterais avoir plus de renseignement concernant la physiopathologie des shunts gauche droite et l’inversion droite gauche et sa traduction a écho et doppler cardiaque merci
Thanks for the fantastic article! Why do you get hepatomegaly in truncus arteriosclerosis?
Very good